
CPC
#2: Tuesday, October 22, 2002
Hurd
Hall, The Johns Hopkins Hospital
12:00 Noon
| Clinical Discussant: | Pam Lipsett, MD |
| Pathologist Resident: | Lori Iaconis, MD |
| Pathologist: | Christine Iacobuzio-Donahue, MD |
| Radiologist: | David Hodge, MD |
| Moderator: | Charles Wiener, MD |
Chief
Complaint:
A 51- year-old man status-post
liver transplant with cough and
dark urine for one week.
History
of Present Illness:
The patient is a 51-year-old African-American
man, status-post orthotopic liver
transplant in 1998 for hepatitis
C that had progressed to end stage
liver disease and portal hypertension.
He presented in May 2001 to an outside
hospital with a one-week history
of cough productive of yellow sputum.
He denied dyspnea, hemoptysis or
chest pain. He also complained of
"dark urine" for one week.
He denied associated frequency,
urgency, or dysuria. He reports
low-grade fever (99.8 F) and chills
intermittently throughout the week.
At the outside hospital, he was
diagnosed with Pseudomonas urinary
tract infection and was treated
with antibiotics (Ciprofloxacin/Zosyn).
He was also found to have elevated
liver enzymes, hyperbilirubinemia,
and increased creatinine. After
two days, he was transferred to
The Johns Hopkins Hospital.
Review
of Systems:
At the time of admission, he had
a mild headache, but no visual disturbances.
He denies sensory or motor disturbances.
There is no abdominal pain, nausea,
vomiting, change in bowel habits,
bloody stools or change in weight.
He denies musculoskeletal pain.
Past
Medical History:
End stage liver disease with orthotopic
liver transplant (07/98)
Diabetes mellitus.
Chronic hepatitis C infection
Sigmoid colonic polyps with histoplasmosis
found on biopsy (08/00)
Nephrolithiasis.
Past
Surgical History:
Orthotopic liver transplant (7/98)
Social
History:
Single, no children; Lives with
parents; Remote history of intravenous
drug use and alcohol abuse (quit
1998); Remote history of tobacco
use (quit 1999); no recent travel
Family
History:
Mother and Father with diabetes
mellitus; no history of CNS, cardiac,
gastrointestinal, pulmonary or hematologic
disease.
Physical
Exam on admission:
Vital Signs:T= 38.0 C; BP= 110/75;
HR= 105; R=18 (97% on RA)
General: in no apparent distress;
well-developed man.
HEENT: sclera and oral mucosa are
very icteric; pupils equal and reactive
Neck: supple; no lymphadenopathy;
no bruit; no JVD
Cardiovascular: no murmurs, rubs
or gallops
Respiratory: lungs are clear bilaterally
Abdomen: abdomen is soft and non-tender;
no masses or organomegaly
Neurological: alert and oriented;
sensory and motor grossly intact
Laboratory
Values on admission:
Sodium 131 mEq/L, Potassium 3.4
mEq/L, Chloride 102 mEq/L, Bicarb
17 mEq/L, BUN 52 mg/dL, Creatinine
2.3 mg/dL, Glucose 377 mg/dL
WBC
5210 cells/mm3, Hgb 9.0 g/dL, Hct
26.1%, platelets 128,000/mm3
Total Bilirubin 16.3 mg/dL, AST
181 U/L, ALT 120 IU/L, Alk phos
207 IU/L
Chest X-ray: no infiltrates, no effusion
Urine: no WBC's, minimal bacteria
Hospital
Course:
Hepatic
biopsy at that time of admission
showed mild to moderate acute rejection
superimposed on chronic hepatitis
C infection. He was treated with
high dose corticosteroids for rejection.
Approximately 14 days into his hospital
course he developed acute on chronic
renal failure and worsening portal
hypertension with increasing ascites.
Corticosteroids 30 mg/d were continued
for presumed rejection. He became
progressively coagulopathic and
thrombocytopenic. He was started
on Vancomycin after methicillin
resistant Staphylococcus aureus
grew from one of three blood cultures.
Paracentesis did not reveal peritonitis.
21 days after admission he developed
hypotension and tachycardia and
he was transferred to the ICU. Blood
cultures were repeatedly negative.
Echocardiogram revealed a pericardial
effusion requiring pericardiocentesis
yielding a sterile exudate. Post-pericardiocentesis
the blood pressure improved but
he remained tachycardic. His condition
continued to deteriorate as he developed
cardiac dysrhymias, declining mental
status, hypoxemia and pancytopenia.
Repeat blood cultures were negative.
Chest X-ray demonstrated bilateral
upper lobe alveolar infiltrates,
focal ill-defined alveolar infiltrates
in the right lower lung, and atelectasis
in the left lower lobe. Bronchoalveolar
lavage revealed no pathogens. Zosyn,
Ciprofloxacin, Vancomycin, and Fluconazole
were administered empirically. Corticosteroids
were being gradually tapered to
10 mg/d. Radiologic studies of the
brain performed to evaluated altered
mental status showed multiple non-enhancing
acute infarctions (see Images 1-5
below). The patient developed multi-system
organ failure and refractory hypotension
expired one month after admission.
Image #1. Unenhanced CT brain: Focal area of low attenuation left basal ganglia appearing since last exam, no evidence of acute hemorrhage (additional areas of low attenuation seen in both cerebellar hemispheres - not shown). Atrophy.
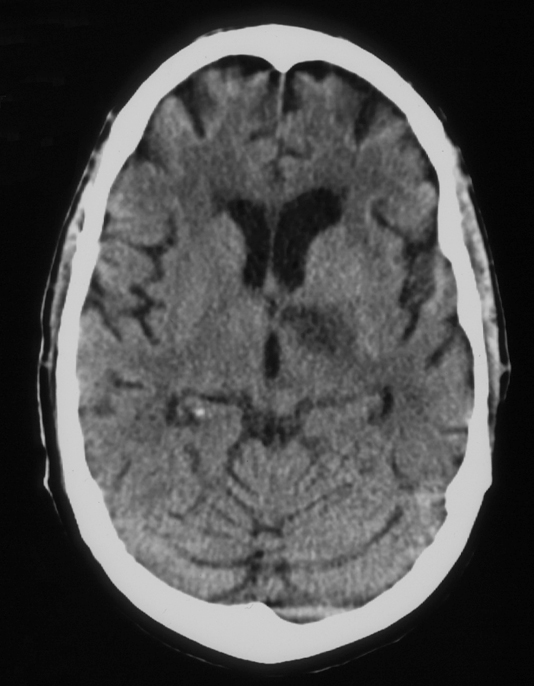
Image #2. MRI brain, FLAIR sequence: Abnormal increased T2 signal left basal ganglia, left posterior limb internal capsule corresponding to CT abnormality. Additional foci are seen; for example, left occipital lobe in this image. Cerebellar lesions demonstrated corresponding to CT abnormality (not shown).
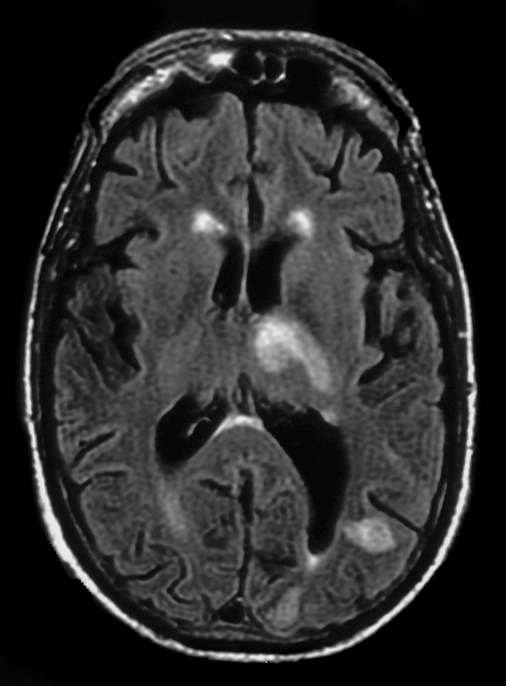
Image #3. MRI brain, FLAIR sequence: Additional lesion right fronto-parietal region.
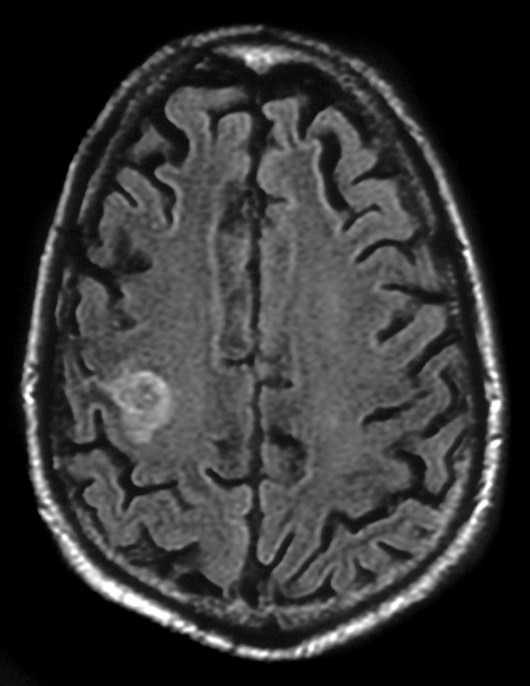
Image #4. MRI brain, diffusion-weighted sequence: Increased signal compatible with acute infarct (confirmed by decreased signal as demonstrated by ADC maps, not shown).
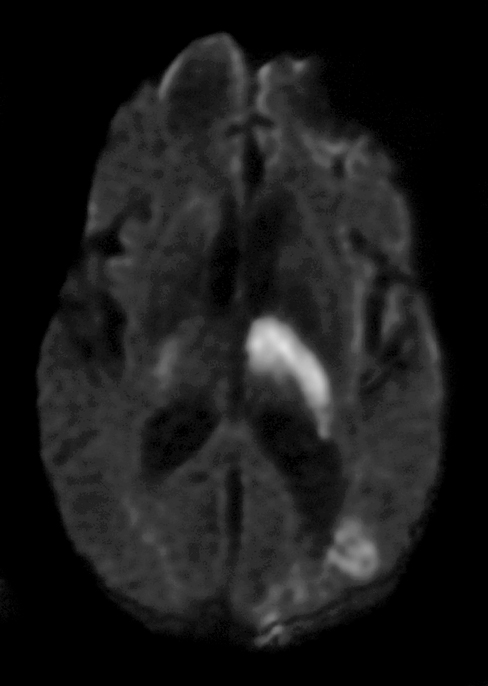
Image #5. MRI brain, diffusion-weighted sequence: Additional lesion compatible with acute infarct.
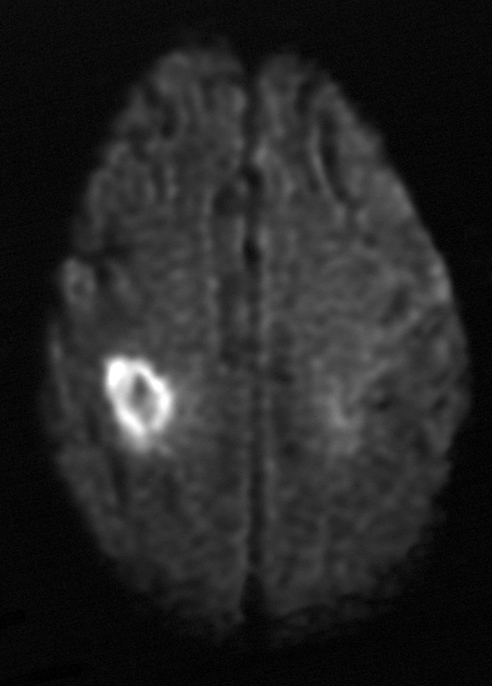
Comment: pre-contrast T1 images demonstrate no evidence of acute hemorrhage, Gadolinium enhanced images demonstrate no evidence of suspicious enhancement, acute infarcts confirmed by ADC maps (not shown).
What is the most likely cause
of death?
| See Answer to CPC #2 |