
CPC
#3: Tuesday, November 26, 2002
Hurd
Hall, The Johns Hopkins Hospital
12:00 Noon
| Clinical Discussant: | Linda Lee, MD |
| Pathologist Resident: | Sharon Swierczynski, MD PhD |
| Pathologist: | Elizabeth Montgomery, MD |
| Radiologist: | Katarzyna Macura, MD PhD |
| Moderator: | Charles Yeo, MD |
Chief
Complaint:
A 52-year-old female with left-sided
abdominal pain and diarrhea.
History
of Present Illness:
A 52-year-old woman developed left-sided
abdominal pain and severe diarrhea
during March of 1999. Her abdominal
pain was cramping and mildly relieved
by food, but not with defecation.
Her diarrhea was watery, she had
>4 bowel movements each day.
There was no hematemesis or melena.
Her symptoms persisted with varying
severity and no relief with over-the
–counter medications. In August
of 1999, she underwent an upper
endoscopy that revealed multiple
ulcers in the stomach and duodenum.
A biopsy for Helicobacter pylori
was negative. She was started on
Omeprazole with resolution of her
abdominal pain and diarrhea.
When the proton pump inhibitor was discontinued several months later, her diarrhea and abdominal discomfort returned. During August of 2000, an upper GI series again demonstrated a duodenal ulcer. A serum gastrin level was normal. Her stool was negative for WBCs, ova, parasites, or C. difficile. An abdominal MRI was reportedly negative. She was restarted on Omeprazole and followed.
During 2002, an abdominal MRI reportedly demonstrated a solitary lesion in the medial segment of the left lobe of the liver. No other upper GI abnormalities were noted by imaging studies. In April of 2002, the patient underwent an unremarkable upper endoscopy at The Johns Hopkins Hospital. No ulcers were seen.
Review
of Systems:
Notable for paresthesias of the
left hand, anxiety, and intermittent
vaginal spotting.
Past
Medical History:
Borderline hypertension and three
normal spontaneous vaginal deliveries.
Past
Surgical History:
She is status post tonsillectomy
and adenoidectomy as a child.
Social
History:
She is married with three grown
children, and works as a homemaker.
She denies alcohol or tobacco use.
She has not traveled overseas in
over 5 years. She lives in a suburban
setting and has no contact with
farm animals or products. She eats
a normal diet.
Family
History:
Her father had cardiac disease and
hypertension, and died of a myocardial
infarction. Her mother is alive
with thyroid disease. Her three
siblings are healthy. There is no
family history of cancer or diabetes
mellitus.
Allergies:
No known drug allergies. No known
allergies to latex.
Physical
Examination:
The patient is a well-developed,
well-nourished white female in no
acute distress. Vital signs reveal
blood pressure 144/83, pulse 85,
respiratory rate 18, O2 sat 99%
on room air, and temperature 35.7?C.
Head and neck exam reveals no thyromegaly
or lymphadenopathy. Lungs are clear
to auscultation bilaterally. Cardiac
exam is unremarkable with no murmurs,
gallops, or rubs appreciated. Abdomen
is soft, nontender, and nondistended.
Rectal examination was normal, with
hemoccult negative stool. There
is no hepatosplenomegaly or periumbilical
adenopathy. Neurological exam is
unremarkable.
Laboratory
Studies:
CBC: WBC 6100/mm3 , HgB 13.6 g/dL,
Hct 39.5%, MCV 90.4fL, RDW 13.4%,
platelets
268,000/mm3
Basic metabolic panel showed the
following results: Sodium 140 mEq/L,
potassium 3.8
mEq/L, chloride 101 mEq/L, BUN 10
mg/dL, creatinine 0.7 mg/dL, glucose
95 mg/dL, bicarbonate 26 mEq/L
Liver function tests demonstrated
the following: Total protein 7.8
g/dL, albumin 4.5
g/dL, total bilirubin 0.5 mg/dL,
ALT 11 IU/L, AST 17 IU/L, alkaline
phosphatase 73
IU/L
Amylase 54 IU/L, Lipase 27 IU/dL
Ca2+ 10.1 mg/dL
CA 19-9 = 40.4 U/mL (1-36)
Radiological
studies at JHH:
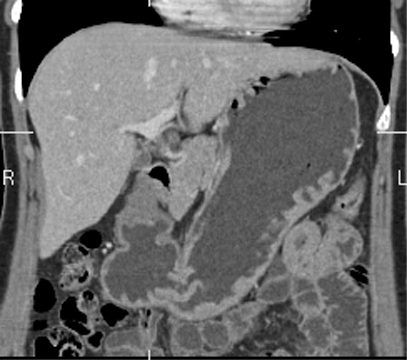
CT scan (Figures 1,2,3)
Figure 1
Coronal reformatted CT image of
the stomach.
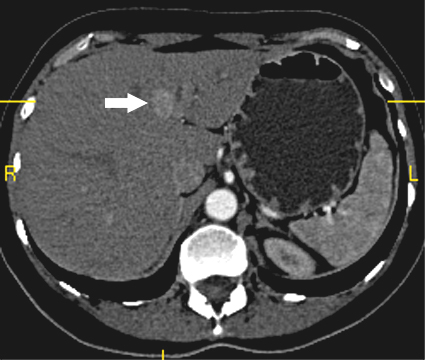
Figure
2.
Axial CT image of the liver, acquired
during the early arterial phase
of contrast injection, shows a 1.2
cm enhancing mass (arrow) in the
left lobe of the liver. Note, the
intense enhancement of the aorta
and poor visualization of the portal
vein, which is characteristic for
the arterial phase.
Figure
3
3D reformatted image of the abdominal
aorta shows a hepatic artery branch
(black arrow) supplying the mass
in the left lobe of the liver (white
arrow).

What is your differential diagnosis?
How would you proceed?
| See Answer to CPC #3 |