
Answer to CPC #4 (Tuesday, December 17, 2002)
This patient presented with shock less than six months after orthotopic heart transplantation. The causes of shock include cardiogenic shock, hypovolemic shock, septic/anaphylactic shock and obstructive shock resulting from pulmonary embolism. This patient clearly has cardiogenic shock, as he presents with tachypnea, hypotension, increased jugular venous pressure, cyanosis and lactic acidosis resulting from hypoprofusion. Echocardiogram is confirmatory in that it excludes tamponade and demonstrates left ventricular hypokinesis.
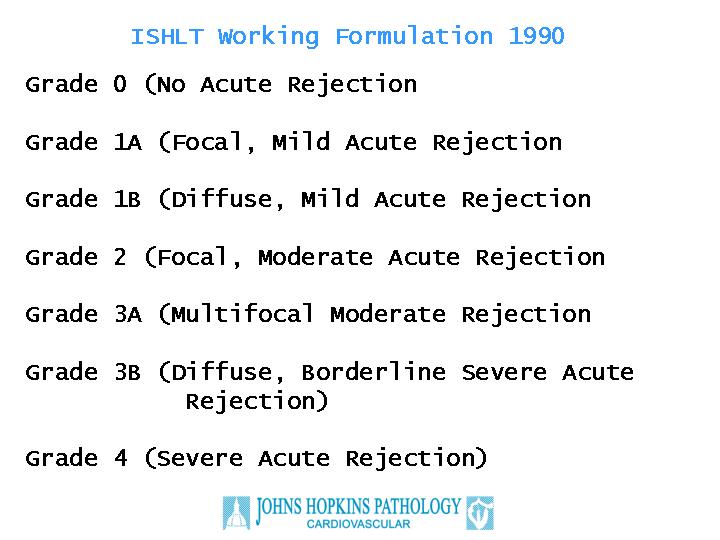
In a patient who has undergone heart transplantation, the main differential diagnosis for cardiogenic shock centers on infection and on rejection. The patient had no evidence of bacterial or fungal infection on blood cultures, and no evidence of cytomegalovirus infection. Rejection can be divided into that caused by cellular and humoral immune responses. Cardiac biopsies are an excellent means to evaluate cellular rejection. Cellular rejection is diagnosed by identifying lymphocytic infiltration of the myocardium accompanying evidence of myocyte damage. The International Society of Heart Lung Transplantation (ISHLT) Working Formulation of 1990 establishes a grading system ranging from grade 0 (no acute rejection) to grade 4 (severe acute rejection), which is used in most centers (Figure 1). In contrast, the ISHLT Working Formulation does not define criteria to diagnose humoral rejection. Humoral rejection is associated with complement deposition and antibody deposition directed against donor antigens located on the endothelial surface of the graft. Risk factors for humoral rejection include a positive donor-specific cross match or preformed anti-HLA antibodies. Pathologically, humoral rejection may be associated with obliteration of the cardiac vasculature, a process known as Coronary Allograft Vasculopathy or Accelerated Graft Arteriosclerosis. However, cardiac biopsies taken to monitor for rejection do not sample these larger arteries, and hence the biopsies may be normal or show the resulting ischemic changes in the myocardium. We therefore should think of humoral rejection when the clinical picture is consistent with rejection, but the biopsies show little evidence of cellular rejection, as was seen in this case. Hence, the most likely pathologic process is that of humoral rejection.
Figure 1
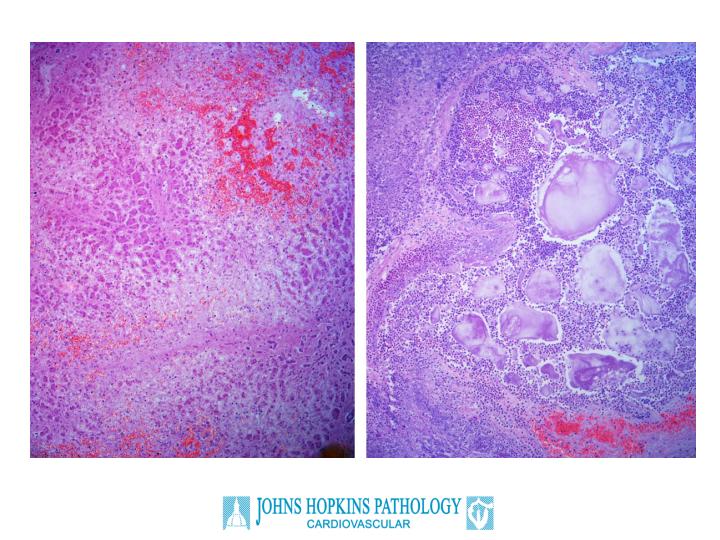
The autopsy confirmed this clinical suspicion. The left anterior descending coronary artery was 90% occluded by intimal proliferation, without a dense atherosclerotic plaque (Figure 2). There was severe vascular rejection of the coronary arteries with an exudative component. Examination of the intracardiac capillaries revealed an endothelialitis characterized by a proteinaceous exudate consistent with severe rejection, although the inflammatory cell infiltrate around the capillaries was only moderate (Figure 3). Other findings of note in the autopsy related to the effects of cardiogenic shock; namely, chronic passive congestion of the liver and acute pancreatitis (Figure 4). The latter findings likely account for the patients' abdominal pain at presentation.
Figure 2
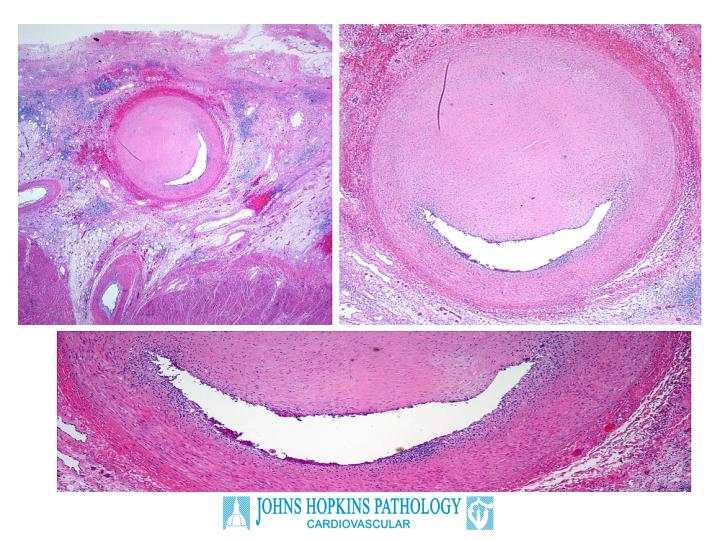
Figure 3
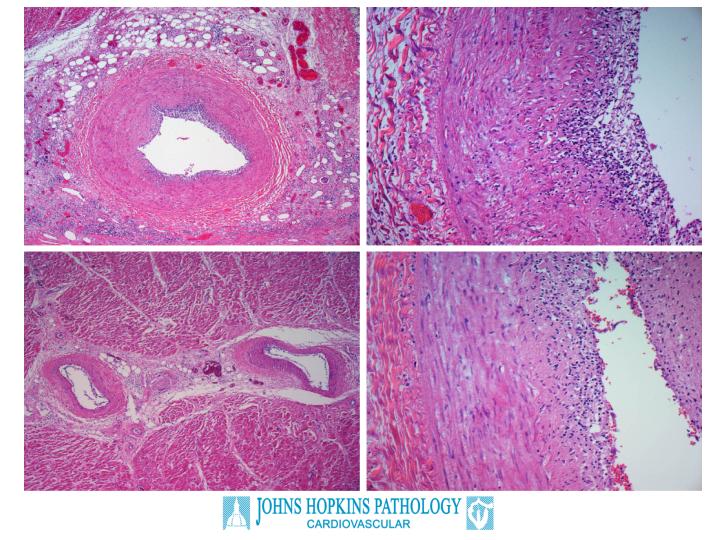
Figure 4
In summary, this patient expired from Coronary Allograft Vasculopathy (Accelerated Graft Arteriosclerosis), which resulted in cardiogenic shock. This is a lesion that is difficult to treat, as it does not seem to be responsive to standard immunosuppressive therapies used to treat the more common cellular rejection. Possible treatments include plasmapheresis, but these are unlikely to be of help in advanced cases such as the one presented.