|
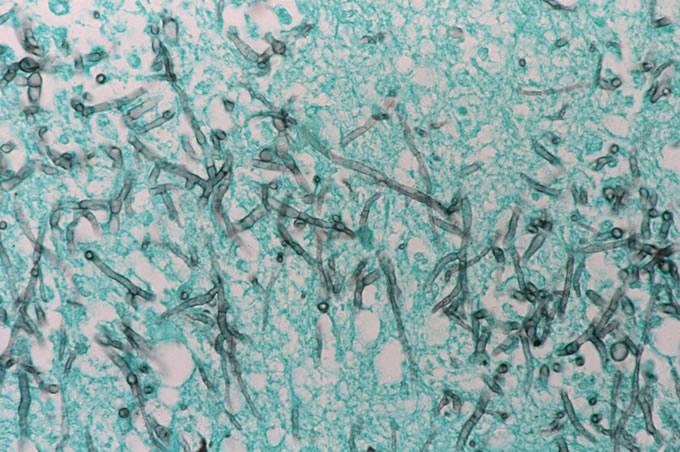
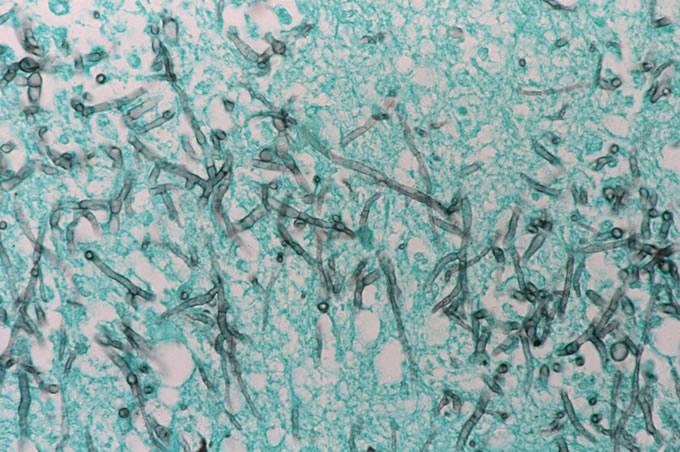
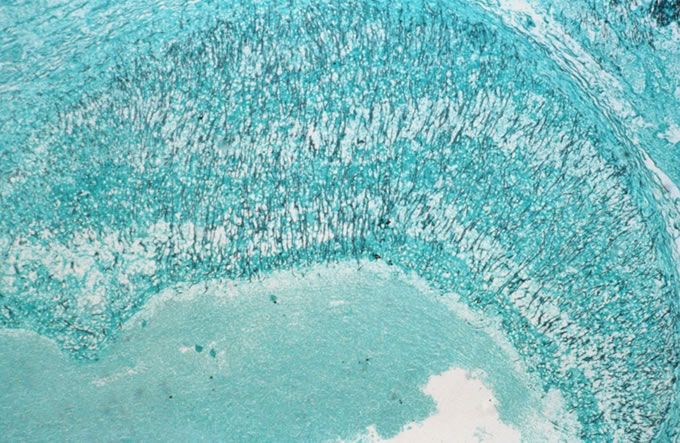
Figure
2: Brain Biopsy, Silver Stain
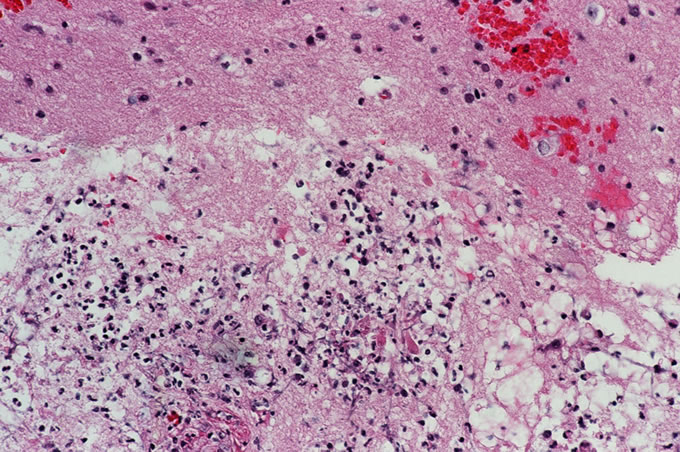
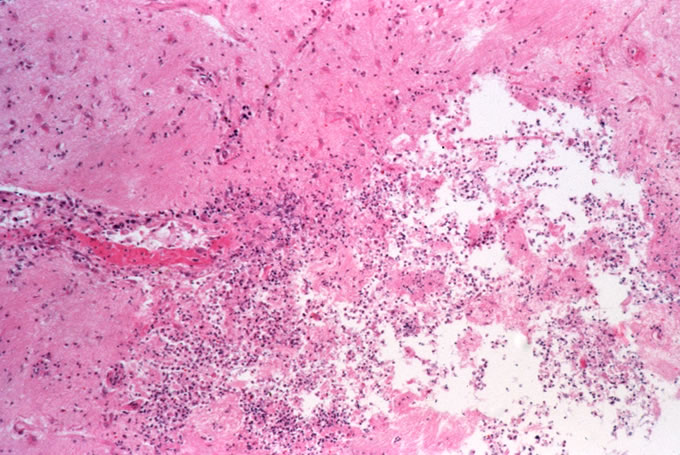
The
patient expired from progressive
neurologic deterioration and
clinical herniation shortly
after the brain biopsy and
a complete autopsy was performed.
Selected images from the autopsy
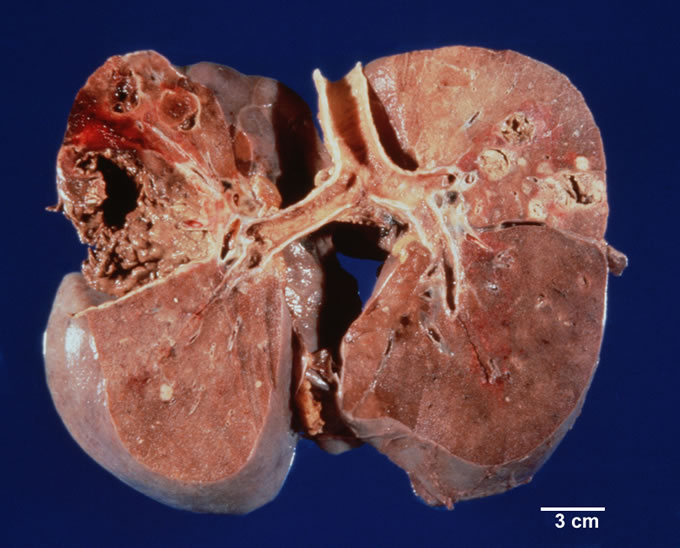
are shown below. The lungs
demonstrated multiple cavitary
lesions, including one large
cavitary lesion in the left
lung (corresponding to the
largest cavity on CT scan)
which eroded the pleura. These
cavities contained numerous
fungal hyphae, and the walls
of the cavities demonstrated
invasive fungal hyphae. The
heart contained a mitral valve
ring abscess, which contained
numerous hyphal forms, and
this represented a portal for
dissemination of fungus systemically.
Numerous fungal abscesses were
documented within the thyroid,
adrenal, retroperitoneal fat,
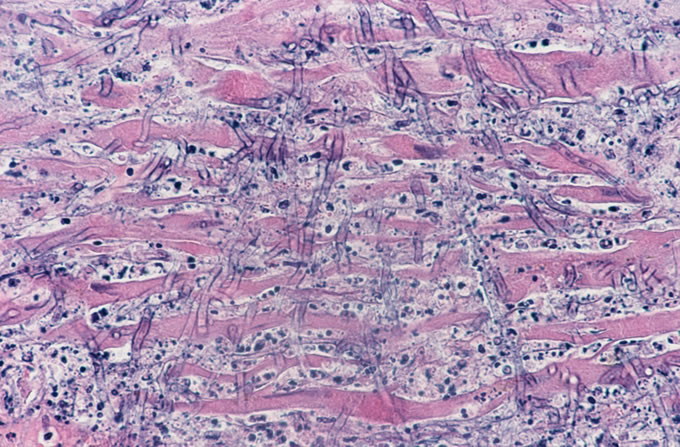
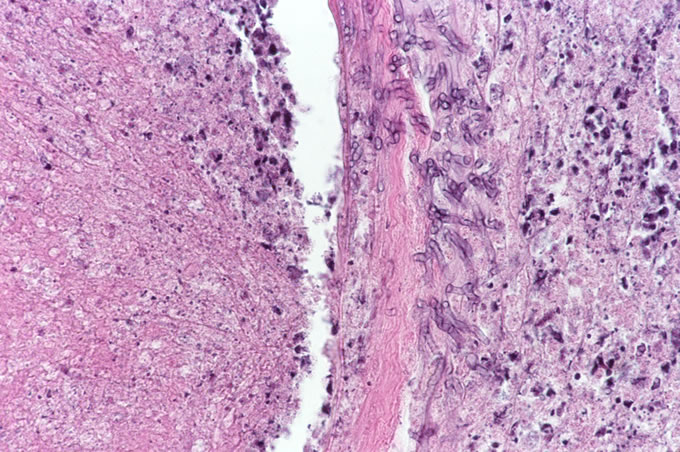
and myocardium. The myocardial
abscess is illustrated below;
note at higher power the fungi
growing over dying cardiac
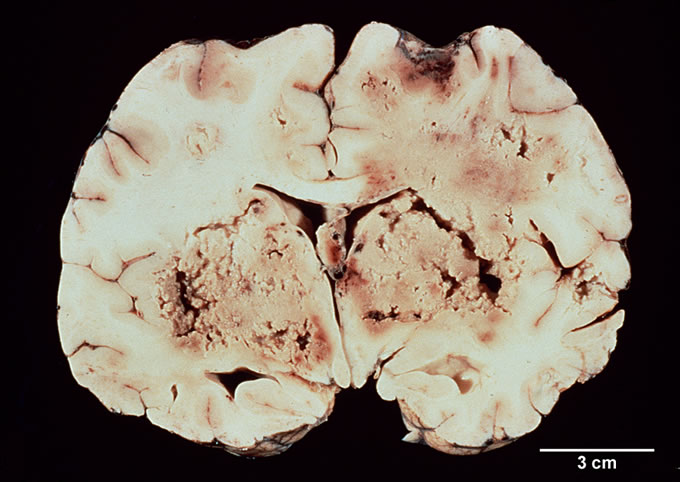
myocytes. Examination of the
brain was remarkable for large
areas of necrosis involving
the basal ganglia with associated
marked cerebral edema, leading
to uncal and cerebellar herniation.
There was additionally external
herniation in the right parietal
occipital area through a craniotomy
site used to perform the diagnostic
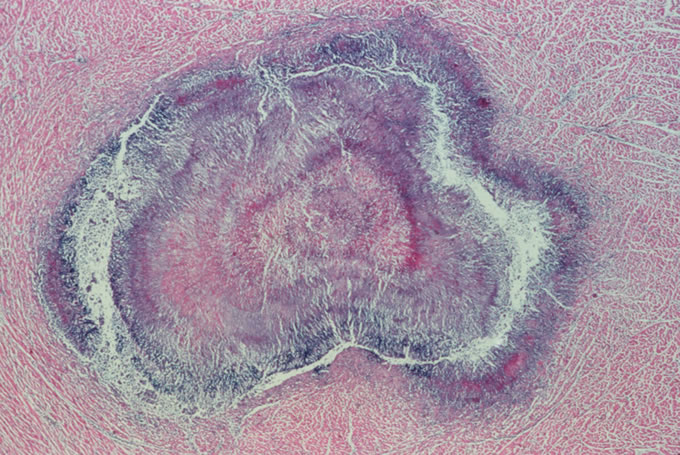
brain biopsy. Histologic sections
of the necrotic areas of brain
demonstrated fungal abscesses.
Sections of meningeal arteries
revealed septic fungal thrombi,
with fungal hyphae extending
out of the blood vessel wall
into the adjacent parenchyma.
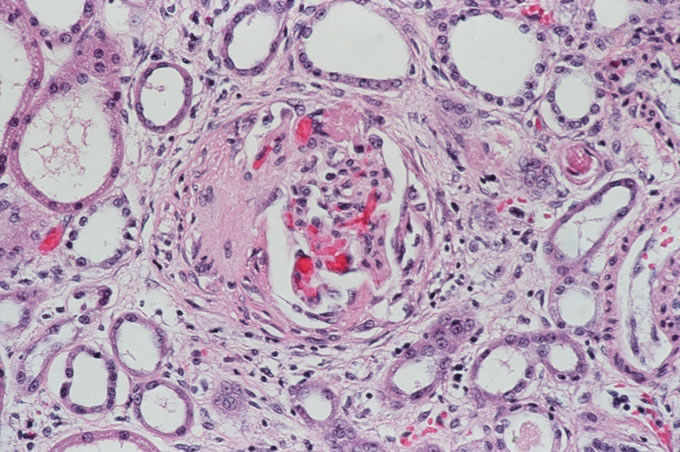
The kidneys demonstrated fibrous
crescents in the Bowman's capsule
of glomeruli, indicative of
prior glomerular damage from
glomerulonephritis. In this
setting, the findings in the
kidney are entirely compatible
with treated, now inactive
Wegener's granulomatosis.
|
|
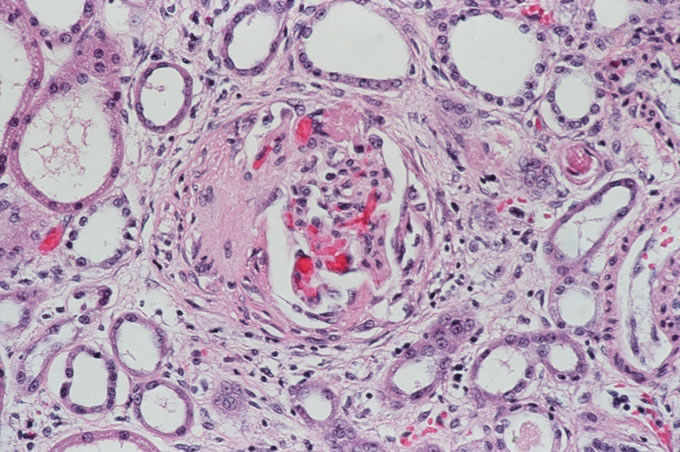
Figure
10: Fibrous crescents within glomeruli
of kidney, indicative of prior glomerular
injury as would be seen in Wegener's
granulomatosis.
This
was an extremely challenging case
to analyze. One important concept
was that the tempo of the patient's
disease changed dramatically in
the last month of life. For three
years prior to coming to JHH, she
had an indolent illness with mild
to moderate renal insufficiency
and mild respiratory findings. Soon
after administration of immunosuppressives,
she clinically declined with worsening
respiratory symptoms and radiographs.
Furthermore, the patient's renal
manifestations of Wegener's improved
on immunosuppressive therapy whereas
the lung lesions did not. In retrospect,
the thickness of the walls of the
cavities on the CT scans, as well
as their large size, are suggestive
that at least some of the pulmonary
findings were not due simply to
Wegener's granulomatosis. Given
the subsequent development of brain
lesions, the differential diagnosis
revolved around infectious causes
of cavitary lung disease associated
with brain lesions.
Possible
etiologies include bacteria,
most specifically Staphylococcus,
anaerobic gram-negative rods such
as E. coli, and mixed anaerobes
acquired from aspiration. Against
this possibility are the patient's
subacute clinical course of decline,
and the absence of cultures revealing
these organisms. Typically bacterial
abscesses present in a more fulminant
fashion. Higher bacteria such as
Mycobacterium tuberculosis
or kansasii lead to cavitary
lung disease frequently, but only
infrequently cause brain abscesses.
Nocardia is a serious consideration
given its proclivity to cause pulmonary
and brain abscesses, but is unlikely
given the fact that the patient
was on trimethoprim/sulfamethoxazole
prophylaxis for pneumocystis; trimethoprim/sulfamethoxazole
will also cover Nocardia. Cavitary
lesions due to Nocardia or Mycobacteria
also typically yield abundant organisms
that would likely have been seen
on a bronchioalveolar lavage specimen.
Viruses and parasites only extremely
infrequently lead to the findings
of cavitary lung disease and brain
abscess.
The
differential diagnosis then turns
to fungal infections; these
can be divided into two categories.
The
first are the primary fungal infections,
which are capable of causing disease
in normal patients and rarely spread
systemically, though they spread
systematically more frequently in
immunosuppressed hosts. These include
Histoplasmosis, Cryptococcus, Coccidioidomycosis,
and Blastomycosis. However, these
fungi rarely cause central nervous
system abscesses, usually present
with a more indolent tempo (chronic
disease), and should have been identified
on bronchioalveolar lavage specimens,
as they are typically abundant in
infectious sites.
The
second are the opportunistic fungi,
which are ubiquitous within the
environment but never pathogenic
to normal hosts. They may persist
for years in the diseased lung of
patients with underlying cavitary
lung disease, but do not invade
unless the patient is markedly immunosuppressed.
These fungi include the Zygomycetes
such as Mucor, Rhizopus, and Absidia,
which typically affect the sinuses
and may spread directly to the brain,
and septate fungi such as Aspergillus,
Fusarium, and Pseudallescheria boydii.
These latter three fungi cannot
be distinguished on histologic sections
and require culture for definitive
identification. The greatest risk
factors for invasive fungal disease
by these organisms are neutropenia
and steroid use. Aspergillus fumigatus
is the most frequent colonizer of
the lungs of patients with chronic
lung disease. The fungal hyphae
of Aspergillus only infrequently
fragment, so that blood cultures
and sputum cultures are frequently
negative, even in the face of disseminated
angioinvasive fungal disease
In
summary, this patient expired from
angioinvasive fungal infection
proven on cultures to be both Aspergillus
fumigatus and Pseudallescheria
boydii. This angioinvasion appears
to have been secondary to immunosuppression
related to Wegener's granulomatosis
and therapy to control this autoimmune
disease.
Return
to Top
|