
CPC
# 4: Tuesday, December 18, 2001
Hurd Hall, The Johns Hopkins Hospital
12:00 Noon
| Clinical Discussant: | Philip
Spevak MD Duke Cameron MD Reid Thompson MD Hal Dietz MD |
| Pathologist: | E. Rene Rodriguez MD |
| Moderator: | Michael Barone MD |
Chief
Complaint:
15 year old girl with unwitnessed
cardiopulmonary arrest and sudden
death
History
of Present Illness:
The patient experienced an unwitnessed
cardiopulmonary arrest in the front
yard of her house and was found
unconscious by a bystander. She
was rushed by ambulance to an emergency
room. She was pronounced dead after
an unsuccessful resuscitation lasting
39 minutes. Down time was estimated
to be 10 minutes.
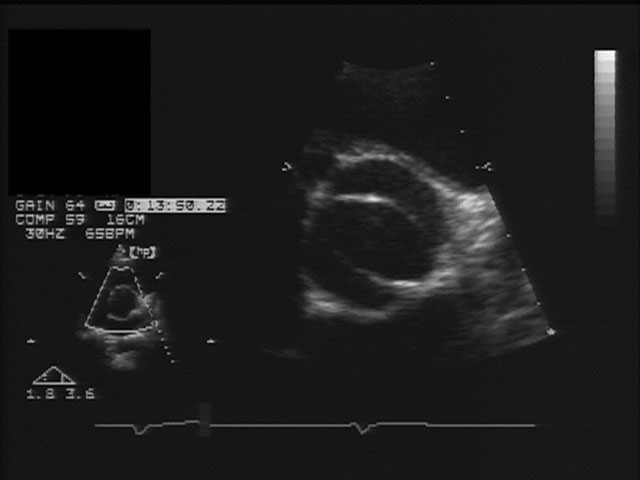
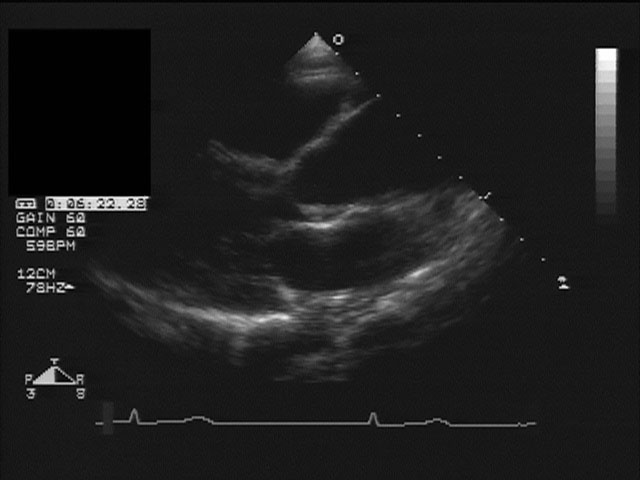
Hypertension was noted at age 14 years during examination prior to sports participation. Referral to a cardiologist resulted in a diagnosis of aortic coarctation. Blood pressure in the right arm was 140/90 and in the lower extremity, 90/40. There was a systolic ejection murmur, which radiated to the back. The auscultory findings heard at the apical location are heard in figure 1. An echocardiogram showed a bicommissural aortic valve (figure 2a is freeze frame of short axis of aortic valve and 2b is freeze frame of long axis of aortic valve and ascending aorta; figure 2c is a short clip of aortic valve motion (Windows Media Player recommended for viewing)).
Figure
2a
Figure
2b
There was no significant aortic stenosis or regurgitation. The coarctation is displayed in figure 3 (on the left side without color Doppler and on the right, with color Doppler).
Figure 3
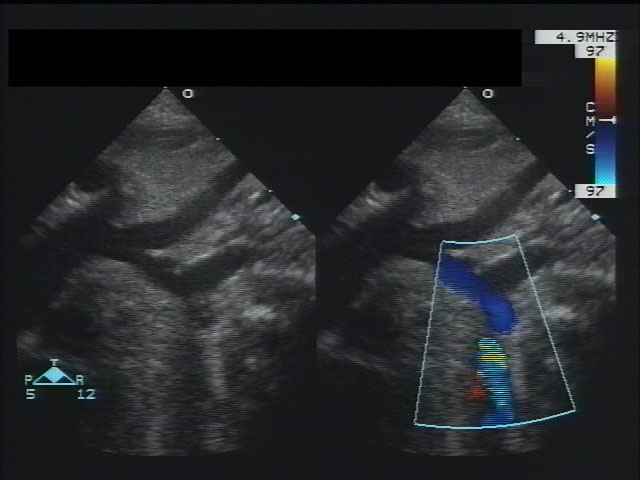
Cardiac catheterization confirmed the severe coarctation of the aorta.
Three months later, a left subclavian flap plasty repair of coarctation was performed and the hypertension resolved. She was discharged with no physical restrictions except to avoid vigorous contact sports. She was instructed to take antibiotics for endocarditis prophylaxis prior to procedures. She continued to play varsity softball.
Her cardiologist saw the patient four times over the next year and a half. On each visit, she was found to be in good health and denied shortness of breath, easy fatigability, headache, chest pain and syncope. An exercise treadmill test was performed which showed no evidence of exercise intolerance, resting or exercise induced hypertension. Her blood pressure was documented to be 120-130/54-80 with no gradient between upper and lower extremities and no detectable murmur. An EKG showed normal sinus rhythm with no ectopy. An echocardiogram was done at one of these visits showed very mild stenosis (maximum instantaneous gradient of 11 mm Hg) and no aortic insufficiency. The left ventricular size and function were normal and there was dilation of the ascending aorta.
PMH:
- Full term with APGAR values were 10 at 1 minute, 10 at 5 minutes
- Mild jaundice as newborn (mother 0+, pt A+, Coombs +)
- Recurrent ear infections - received tympanostomy tubes under anesthesia at age 7 years.
- Mild intermittent asthma
- There
was no history prior to death
of unexplained febrile illnesses
or of drug use.
Family
Hx:
No family history of aortic valve
disease or coarctation, high frequency
sensory-neural hearing loss, premature
sudden death, cardiomyopathy, or
connective tissue disease.
Immunizations:
Up to date
Allergies:
Sulfa antibiotics
Physical
Exam:
The following physical was documented
shortly before the episode of sudden
death.
Alert and cooperative teenager in no distress. The height and weight were near 95th percentile for age. There was no cyanosis. The right brachial and right femoral pulses were readily palpable. There was no demonstrable blood pressure gradient measured between the upper and lower extremities. Blood pressure in right arm measured 110/60. The lungs were clear with good air entry. Well-healed thoracotomy scar. The precordium was quiet. S1 and S2 were normal. There was a grade I/VI systolic ejection murmur at the right upper sternal border with no radiation to the back, no diastolic murmur. There was no hepatomegaly. The neurological exam was grossly intact.
Electrocardiogram (figure 4)
Figure
4
Labs:
Wbc 16.9, Rbc 4.67, Hgb 13.6, Hct
40.3, Plt 185,000
Sodium 139 mEq/dl, potassium 4.1
mEq/dl, BUN 12 mg/dl, Creatinine
0.8 mg/dl, Ca 8.7 mg/dl
Questions to consider:
- What
are possible etiologies for
this patient's sudden death?
Consider both cardiac and non-cardiac
causes.
- Would additional diagnostic tests have been helpful for this patient and her family members? If so, what tests would be appropriate?